Medicines and Vaccines Part 3: Is it the Water or the Vaccines?
In this last part of our medicines and vaccines series, we’re going to talk about how vaccines work and how we know they do. I know that vaccines are a contentious topic and I want to start by acknowledging that sometimes delaying or forgoing a vaccine is the evidence-based decision. If someone is pregnant, they shouldn’t have the varicella (chickenpox) vaccine. A child with leukemia probably shouldn’t get the measles, mumps, and rubella (MMR) vaccine. Those conditions which make vaccines temporarily or permanently unsafe for an individual are, thankfully, very, very rare. For most humans, following the CDC vaccine schedule is safe and will provide both them and their contacts with protection against those diseases.
This post is a little more science-y than others have been, though I've tried to keep things as simple as possible. If any of the terms or other information in this piece is confusing, please feel free to contact me and we can discuss it together. No question is unwelcome and I promise to make time to be helpful.
“It’s overloading their immune system.”
I will confess that I used an alternative schedule for Rónán. I had never studied public health and was concerned that I would be “overloading his tiny immune system” unnecessarily, particularly since I stayed home for the first 18 months of his life (no childcare) and exclusively breastfed him. If we have a second child, though, I will confidently breastfeed that little baby through each of their vaccines according to the CDC’s schedule.
I hear concern sometimes from other mothers (and members of the public) that the current CDC vaccine schedule is “too much too soon” and that a child’s immune system can’t handle the stress of it. People will often compare the 1983 vaccine schedule (10 doses) to the current one (~39, depending on how you count). While, yes, that is a lot of pokes in the arm or thigh, the comparison isn’t apples-to-apples and, even if it were, it would still be a bit disingenuous.
We prevent more diseases than we used to and that’s a good thing. Rotavirus is responsible for half a million deaths each year among children under 5 and is the leading cause of hospitalisations for children in the United States under 5. [1] Varicella (chickenpox) was a common infection when I was a child, but now has an effective vaccine. Chickenpox complications include bacterial infections from the sores, pneumonia, encephalitis (infection leading to swelling in the brain), dehydration, and sepsis (an infection in the blood which can be very serious and require hospitalisation). [2] Tetanus, measles, dypyheria, mumps, pertussis, and Hib are all awful diseases. It is good that we don't have to get them and fantastic that, if we do get them, we are less likely to be hospitalised or have severe complications.
But the icing on the Communicable Disease Prevention Cake is this: not only are we preventing more of these diseases, but we're also doing it more efficiently than we were. We’re constantly improving how good our vaccines are–not just in efficacy, but also in safety. We’re exposing children to far fewer antigens with each vaccine than we used to, reducing the (already quite low) amount of stress on your little one’s immune system. What’s an antigen? Antigens are the part of a vaccine that makes your immune system react and learn to recognise and fight a pathogen (germ). It’s against the specific antigen that your immune system produces antibodies. When you have an immune reaction (we’ll talk more about this in the next section), it’s the antigen that your immune system is fighting. Strep throat will expose a child to approximately 25-50 antigens. A cold is about 10. [3]
So, how do the 1983 and contemporary vaccine schedules match up? The current vaccine schedule exposes children to approximately 315 antigens by their 2nd birthday. [3] That 1983 vaccine schedule with just the 10 doses? It exposed children to approximately 3,000 antigens by their first birthday and approximately 12,000 by their 4th birthday. [4] That still isn’t too much for a child’s immune system to take, but it’s certainly more stressful than the 315 we’re throwing at kiddos now. We may be getting more pokes, but we’re throwing fewer mock attacks at our immune system in the process.
“The flu vaccine gave me the flu.”
I think we’ve all heard this one. You dutifully go in for your annual (yes, you need it every year) flu shot and the next day you have a sore arm, a sore throat, and just want to Netflix and chill with your cats. (Or maybe only I binge on tea and Netflix with my cats?) Your doctor insisted that the flu vaccine can’t give you the flu, but then why do you feel so darn awful?
The short answer is that your immune system is fighting off a dead (or dramatically weakened to the point that it couldn’t do anything but look menacing) flu virus that it doesn’t realise is dead (or otherwise useless), so Team You is giving it all it’s got. Your immune system is a tricky beast and some of the things that feel worst—like a fever—are actually your own body trying to cook out the enemy.
When my son was a baby, a friend told me to remember that “[low grade] fevers are your friend” and to not rush to suppress every tiny one since they’re often the sign of a healthy immune system going to work. The fever and fatigue certainly don’t feel nice, but they’re much better than a full blown case of the flu, which usually lasts for a couple of weeks.
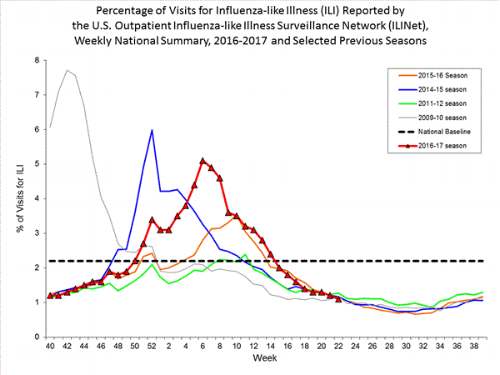
Another possibility why you may feel under the weather after getting a flu shot is that you were exposed to another respiratory illness in the days before you got the shot and now you’re sick with that. Coincidences like that are unfortunate, but do make sense with the timing of when respiratory diseases really kick off. Above is a time series graph showing the number of visits to an outpatient healthcare provider for influenza-like illness (ILI) each week from 2015-present (as reported to ILINet).
Week 40 is generally around the first week of October and the time that we consider the “beginning” of flu season. This is also just about when people start receiving their flu shots (though you can get them earlier). This is also the time when you’re likely to have been near someone sneezing on the bus or in your office, or touched something that was recently touched by someone with poor hand washing habits. It feels unfair to show up, get a poke, and then still get sick, but sometimes “random looks clumpy” (as my coworker often says).
“If one dose wasn’t enough, why would a booster do anything?”
As though a sore arm wasn’t enough once, for some vaccines (e.g., DTaP, MMR, HPV, and rabies) multiple doses are necessary to achieve the necessary immunity. Leading to the common question: if one dose wasn’t enough, why would a second (or third) do the trick? The answer may feel a bit familiar if you’ve ever studied a new language or practiced a new skill. When your immune system meets a new threat for the first time, it has to learn how to defeat it and each meeting after that is stronger and more effective. When I was first learning Latin as a youngster, it took me ages to memorise all the batty grammar charts and I could only recite them very slowly and with many mistakes. But after 9 years of torturing myself with Horace, I can still rattle off my -us, -a, -um chart and a few Catullus poems (in meter no less). Your immune system is like Adolescent Amanda in that way; the more times it meets a pathogen, the better it is at fighting it.
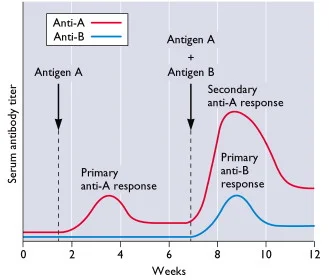
The graph above shows a sample immune response (antigenic response) to two different pathogens. When Team You meets Antigen A for the first time, there’s a small immune response to it, but the second time your immune system encounters it, there’s a much larger response. For both types of learned (“adaptive”) immunity there’s a battle and you would perhaps feel ill for a short time, but much less so with each time your immune system encounters it. We see this with so called “natural immunity” (immunity gained by properly getting sick with a disease), but with that, you’re fighting an immunological enemy at full strength. There are some exceptions to this, like the antibody-dependent enhancement (ADE) we see with dengue infections, but, by and large, boosters work to provide better immune response the same way that doing all those exercises in high school made me better at Latin.
“If people in [Poor Country of Choice] just washed their hands and had clean water, they wouldn’t have [Vaccine Preventable Disease of Choice].”
This (non) question perhaps the one that makes me most uncomfortable. While it is certainly true that some diseases (like norovirus and giardiasis) are spread through water, it is not true that clean water will magically wipe away all communicable diseases, if for no other reason than that some of them (like measles) are primarily spread through the air.
A fantastic example of this is polio. Polio is an enterovirus that is spread through water contaminated with stool (poop). Polio is now almost eradicated, [5] but that wasn’t the case 75 years ago. The United States has been polio-free since 1979, but the United States started chlorinating our water in 1908. [6] Bangladesh, in contrast, has very, very, very poor water quality but was certified polio-free in 2014. [7] So what happened between 1908 and 1978 in the United States and has happened without clean water at all in Bangladesh? The answer is that a man named Dr. Jonas Salk created a vaccine for polio and made it freely available so that every human could be free from the disease.
Dr. Salk’s vaccine trials began in 1955 and it wasn’t long before parents were lining up around city blocks to get the vaccine for their children. The vaccine worked quickly to make the United States polio-free, but there are still areas that have polio circulating.
Why? The only areas which still have wild polio are those which are wracked by war (Pakistan, Afghanistan, and Nigeria). Vaccines have to be kept at very specific temperatures to be effective, which is no trouble in places with consistent electricity, but it makes delivering the vaccine to more remote and impoverished areas expensive and challenging. Securing clean water in the most rural areas of the world is clearly a priority and I would never suggest otherwise, but it will make little difference on its own to wipe the last of polio off the planet.
For measles too, clean water makes little difference in the spread of the disease. Measles is fantastically easily spread—a room in which a contagious person has been continues to harbor the virus for hours after the person has left, leaving anyone not immune vulnerable should they come into it. [8] Measles offers the additional challenge of being contagious before symptoms appear, so a person who feels well can be passing it to others without any knowledge. This makes investigating and controlling outbreaks challenging because a person unknowingly ill may take an airplane or attend a concert and spread the disease in those close quarters. I dearly wish that engineering solutions were all that public health issues need, but as I discussed in Health: More than Healthcare, our health is made up of many intersecting factors and one of them is actual medical care.
Glossary
- Antigen–a toxin, germ, or other foreign substance that triggers an immune response.
- Traditional Vaccine Types
- “Killed” (also called “inactivated”) vaccine–Pathogen (germ) was previously living, but was destroyed. Must be accompanied by an adjuvant to stimulate an immune response (e.g., polio, cholera).
- Live, attenuated–Pathogen is alive, but weakened (e.g., measles, yellow fever)
- Related non-pathogenic agent–A pathogen related to the one to which immunity is desirable (e.g., using cow pox to stimulate immunity to smallpox).
- Subunit–Introduction of a smaller unit of a pathogen to stimulate an immune response (e.g., HPV vaccine).
- Rotavirus in the US. Centers for Disease Control and Prevention. 2016. https://www.cdc.gov/rotavirus/surveillance.html
- Varicella Complications. Centers for Disease Control and Prevention. 2016. https://www.cdc.gov/chickenpox/about/complications.html
- Multiple Vaccines and the Immune System. Centers for Disease Control and Prevention. 2016. https://www.cdc.gov/vaccinesafety/concerns/multiple-vaccines-immunity.html
- Offit, P., Quarles, J., Gerber, M., et al. Addressing Parents’ Concerns: Do Multiple Vaccines Overwhelm or Weaken the Infant’s Immune System? Pediatrics. 2002;109(1):124 http://pediatrics.aappublications.org/content/109/1/124
- 10 facts on polio eradication. World Health Organization. April 2017. http://www.who.int/features/factfiles/polio/en/
- A Public Health Giant Step: Chlorination of U.S. Drinking Water. Water and Health. http://www.waterandhealth.org/drinkingwater/chlorination_history.html
- WHO South-East Asia Region is officially certified polio-free. World Health Organization. http://www.searo.who.int/entity/campaigns/polio-certification/en/
- Transmission of Measles. Centers for Disease Control and Prevention.